Carpal tunnel syndrome
What is it?
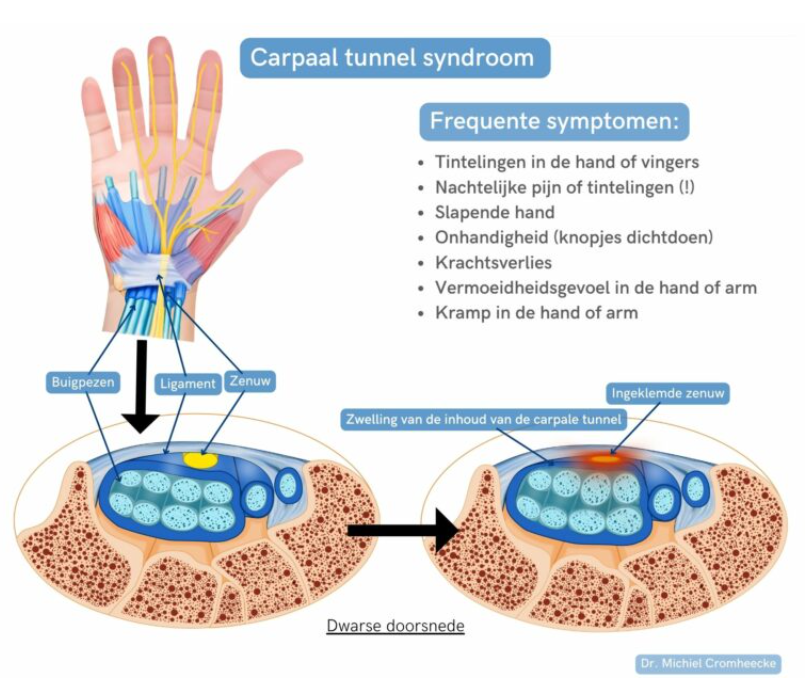
What is it?Carpal tunnel syndrome is caused by an entrapment of the carpal nerve or median nerve in the carpal tunnel. The carpal tunnel, or wrist canal, is bounded at the bottom by the wrist bones and is covered on the top by the transverse carpal ligament. It is a very frequent condition and occurs in about 5% of the population.
Symptoms
Symptoms- You notice tingling and numbness in the fingers or hand. Usually, these tingles are felt in the index finger, middle finger, ring finger or thumb.
- You experience pain or a burning sensation in the aforementioned fingers or thumbs. In some cases, this pain radiates to the forearm. Preventing nightly pain is a very typical treatment objective for carpal tunnel syndrome.
- There may be weakness in the muscles of the hand, resulting in a loss of grip strength. Some people have difficulty performing fine motor tasks (e.g. buttoning).
- Some patients may experience mainly a swollen hand or cramps throughout the hand, especially at night or during work.
Cause
CauseThese symptoms can develop gradually and result from pressure on the carpal nerve in the carpal tunnel.
Often, no specific cause for carpal tunnel syndrome is found. Most people do have a genetic predisposition. Endocrine and metabolic disorders, such as thyroid disease or diabetes, are found to be the cause in some people.
Carpal tunnel syndrome can also occur acutely, for example, after trauma or swelling in the wrist.
Continue reading about this below the image.
Diagnosis
DiagnosisYour physician will diagnose the condition through a combination of clinical tests and positive elicitation tests.
The diagnosis can be confirmed with an EMG or conduction study, but keep in mind that up to 20% of EMG tests can produce false-negative results.
If there is any doubt, specialised ultrasound can be performed to visualise the nerve constriction.
Treatment
TreatmentCarpal tunnel release is a surgical procedure that is performed to relieve pressure on the median nerve in the carpal tunnel. This procedure is considered when non-surgical treatments do not provide sufficient relief for symptoms.
Our team offers three surgical techniques. All these procedures are carried out via day hospitalisation and are performed under local or regional anaesthetic. If you prefer general anaesthesia, this is possible, but it will extend the duration of your stay on the day of the procedure.
This is the most classic procedure for carpal tunnel surgery, and it is still the most commonly performed worldwide. The surgeon makes an incision in the palm of the hand (approx. 3 to 4 cm long) over the carpal tunnel ligament. The surgeon carefully opens the ligament so that the middle nerve is no longer pinched. The surgeon then closes the skin with some sutures. You will be given a hand bandage. After surgery, you may move your hand immediately.
The hand surgeons at Maria Middelares are highly experienced in this minimally invasive surgical technique. With this less invasive method, a small hole is made in the skin of the wrist crease. The carpal tunnel ligament is then opened from the inside (using a camera) with an endoscopic blade. Afterwards, the skin should not be closed with sutures. The wound heals on its own after a few days. After surgery, you may move your hand immediately. This technique is characterised by a very rapid recovery of the patient.
This technique is the least invasive of the three surgical techniques. The procedure is done through a minimal incision in the wrist crease, which requires no sutures afterwards. However, not everyone is eligible for this type of surgery. This can be discussed with your physician during the consultation.
Preparing for your admission
Preparing for your admissionTo assess your health status before the procedure, you need to complete a questionnaire. Your attending physician will decide with you whether to do this through the pre-admission desk at the hospital or through the digital patient platform MyHospital.
Two working days prior to your procedure, a hospital staff member will call you to inform you what time you are expected at the hospital.
Day of your admission
Day of your admissionThe procedure requires a day admission. That means you can return home on the same day and do not have to overnight at the hospital.
On the day of your admission, come to the hospital at the appointed hour having fasted and sign in with your identity card via one of the e-kiosks in the atrium (entrance hall).
You get a ticket via the e-kiosk with a tracking number on it that is shown on the digital screens in the waiting area. A staff member will complete your file and you will receive an identity bracelet with your last name, first name and date of birth. After that, your admission will continue through the OR reception lounge.
You will be prepped for surgery in the operating facilities. The procedure is usually done under local anaesthetic. The anaesthetist will visit you to administer this. Feel free to ask any further questions you may have about the anaesthesia or the procedure.
After the procedure, you will be taken to our pleasant recovery lounge. The nurse will checks your vital parameters while you rest and recover from the surgery. This procedure promotes a quick and smooth discharge, allowing you to leave the hospital easily.
Aftercare
AftercareAfter the surgery, you will be given a hand bandage. Three to five days after the surgery, you can remove the hand bandage. Then, be sure to cover the wound with a simple plaster.
- Open carpal tunnel release: the sutures will be removed 12 to 14 days after surgery.
- Endoscopic carpal tunnel release: the wound heals on its own after a few days.
Move your fingers immediately after surgery. You can quickly use your hand again for simple tasks. We do recommend refraining from lifting heavy weights with the operated hand for four weeks, especially with a flexed wrist. Also avoid tugging on things with your fingers.
Tingling in the fingers improves in most patients fairly soon after the procedure. The palm and scar can sometimes remain sensitive for up to three or four months after the procedure. It can also take this long for the strength in your hand to fully return. In severe cases, the nerve functioning may only improve more than a year later. Complete recovery does not always occur. Therefore, do not delay treatment for too long.
Possible complications
Possible complicationsA compression bandage or cast may be applied to prevent excessive swelling. If the above advice does not help, you can loosen the elastic bandage or remove the hand bandage. The elastic bandage in an open cast can also be loosened.
The post-operative hand bandage will absorb any potential bleeding. Elevating the hand and applying ice can also help. Anti-inflammatory medication is possible, but it must be taken in consultation with your physician.
This complication occurs very rarely, but it occurs more frequently in smokers and diabetics. Contact your physician or the A&E in case of sharply increasing pain, fever (>38.5°C), a festering wound or increasing and spreading redness.
Very rarely, a temporary loss of sensation in the fingers may occur.
- Open carpal tunnel release: in 0.49% of patients
- Endoscopic carpal tunnel release: in 0.19% of patients
Wound healing
Wound healingHere are some guidelines to make your recovery as smooth as possible. If you have any other questions, do not hesitate to contact your attending physician or team.
You had an incision of approx. 3 to 4 cm in length on the palm of your hand. This was closed by sutures and covered with a hand bandage.
You may leave this hand bandage in place until your first follow-up appointment.
The sutures should be removed 12 to 14 days after your procedure. You can contact your GP for this.
You can shower after your first check-up with a water-resistant patch.
The procedure is performed with a minimal incision of about 1 cm. The incision is made following Langer's skin lines, which ensures minimal scarring.
This incision is left open and covered with a hand bandage. The advantage of this is that any post-operative bleeding can be naturally absorbed by the bandage, and there will be no need to remove sutures.
Your bandage may remain closed until your first check-up, after which it will be replaced with a waterproof plaster. This plaster can remain in place for up to 10 days after the procedure and should only be replaced if it becomes soiled or comes loose.
If there is increasing redness or persistent wound fluid, or if you have concerns about your wound, contact the Orthopaedic Secretariat or your GP for a wound evaluation.
Mobilisation
MobilisationIt is very important to move your fingers and thumb as normally as possible after the procedure. To do this, close your hand completely with the fingers pushed into the bandage. Afterwards, stretch the fingers again.
This ensures good circulation and has a beneficial effect on pain. It is normal for this to feel stiff for the first few hours and days after your procedure.
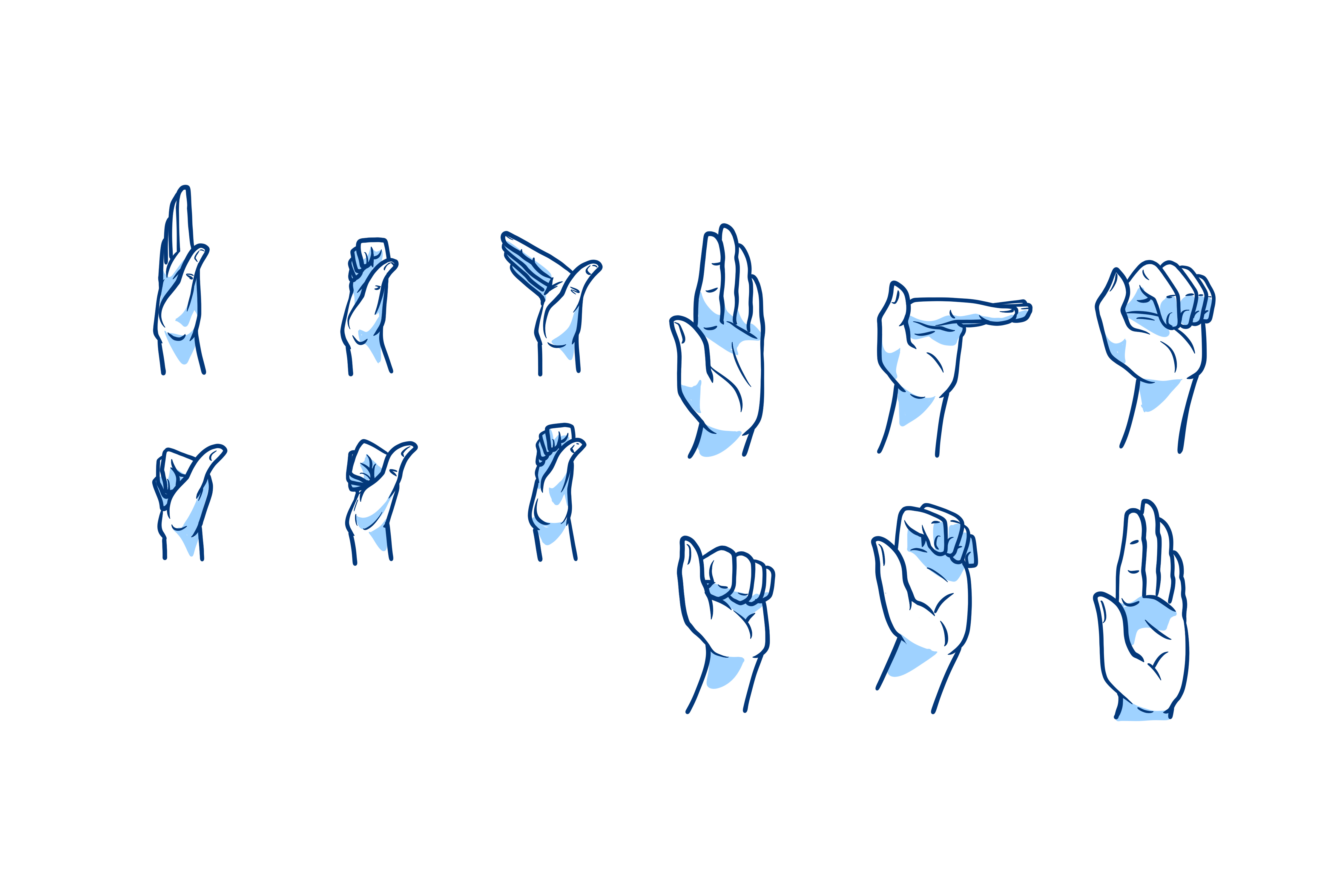
Nerve gliding exercises should be performed to prevent nerve adhesion in the post-operative scar tissue.
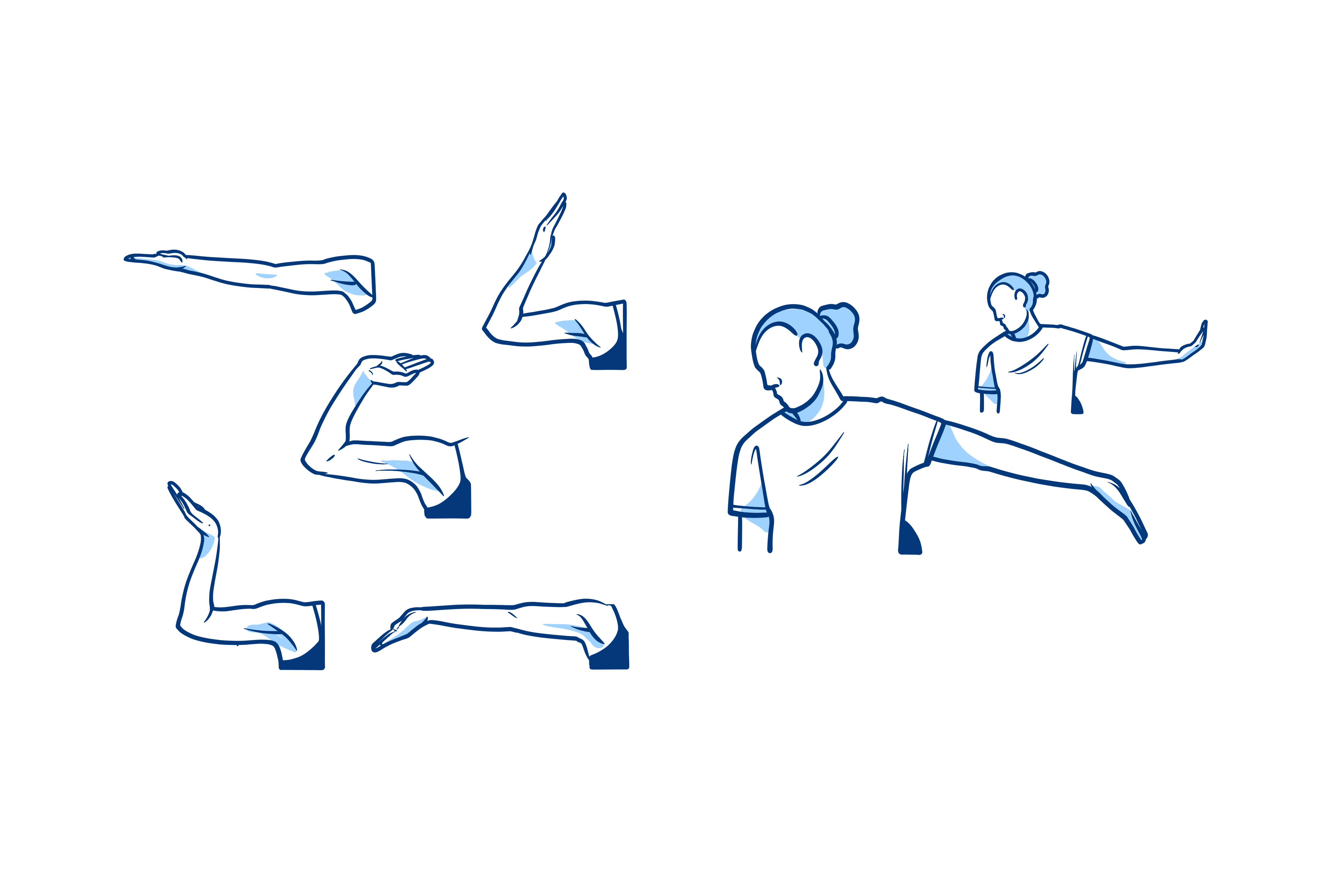
A good exercise involves stretching the arm and bringing the hand back until you feel the nerve stretch into the fingers. Simultaneously turn your head to the other side for maximum stretching.
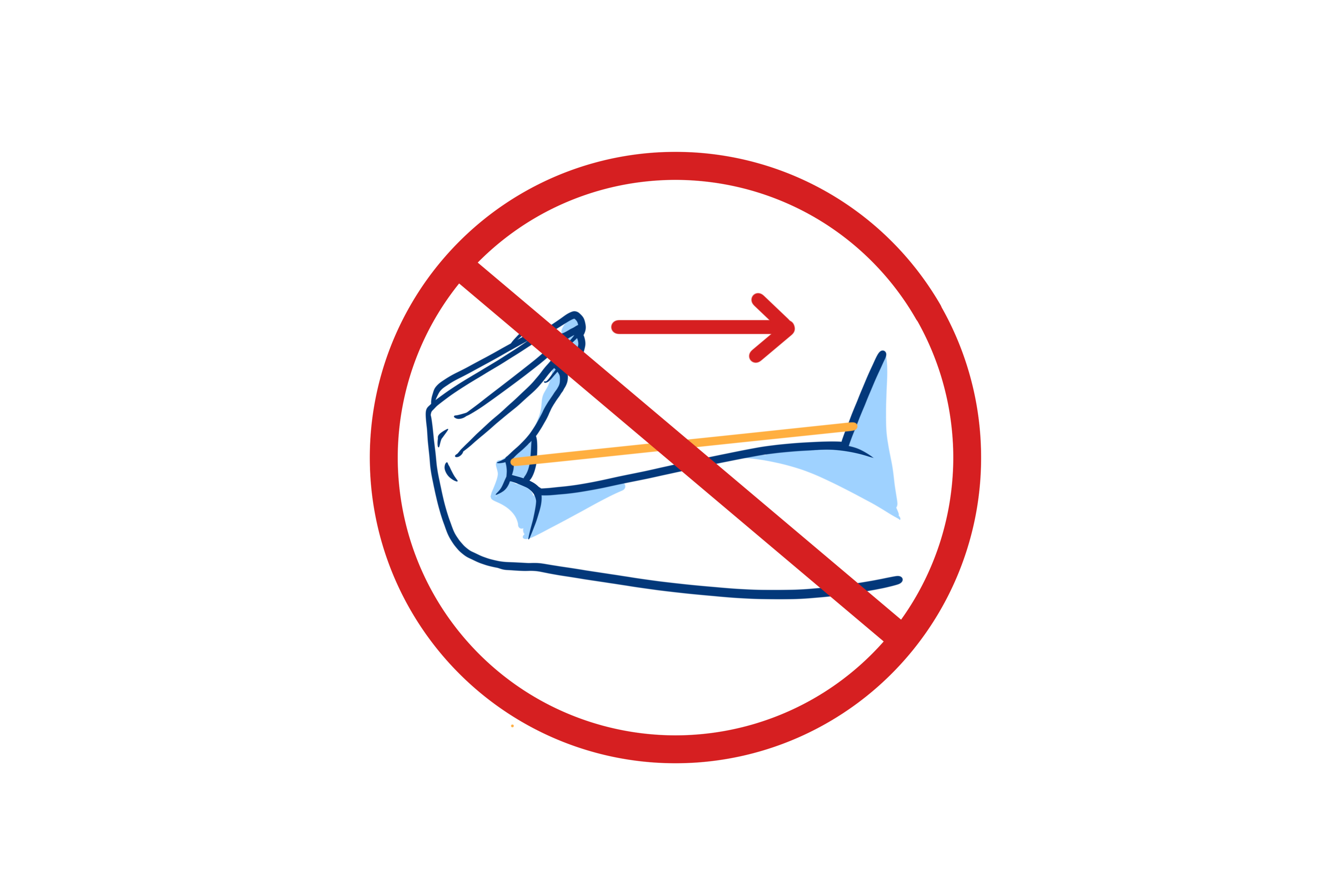
As mentioned earlier, rapid mobilisation is crucial to your rehabilitation. Still, there are some limitations, namely combined forceful bending movements of the wrist and fingers. These can cause a sharp pain because the flexor tendons can get caught between the split carpal ligament.
An example of this movement is carrying a heavy shopping bag or intimate hygiene after going to the toilet. For these tasks, it is best to use your other hand.
These movements should be avoided for 4 weeks.

Expected course of recovery
Expected course of recoveryThe (night-time) tingling and numbness in the fingers usually disappear immediately after the procedure.
In cases of severe or long-standing nerve entrapment, tingling or sensory disturbances may persist for a long time. The nerve needs more recovery time in this case. This can take at least four to six months. In extreme cases, there is irreversible nerve damage.
In 44% of patients, sensitivity in the palm and base of the thumb (known as pillar pain) may develop after some time. This is a normal phenomenon and is due to the healing process. This annoyance disappears spontaneously after four months.
Hand strength typically normalises within three to four months after nerve recovery.
Brochures postoperatieve richtlijnen
Brochures postoperatieve richtlijnenTreatment centres and specialisations
Treatment centres and specialisationsLatest publication date: 15/11/2024
Something wrong or unclear on this page? Report it.






