Cancers of the large intestine
Symptoms and causes
Symptoms and causes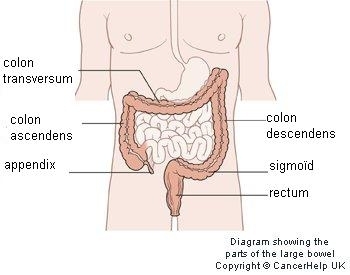
The large intestine
The large intenstine consists of:
- the colon
- consisting of an ascending part (ascending colon), transverse part (transverse colon), descending part (descending colon) and sigmoid
- the rectum
- the sphincter (anus)
The large intestine is part of the digestive tract: food is digested in the large intestine; water and other substances are absorbed and then exchanged with blood. Undigestible parts and waste products are disposed of.
What is cancer of the large intestine?
Colon cancer almost always develops as an intestinal polyp. A polyp (adenoma) is a protrusion or a thickening of the muscoa that lines the inside of the intestine. Polyps are benign tumours, but some of them can grow into malignant tumours. Most colon tumours are made from glandular cells (adenocarcinoma). Within the group of large intestine cancers, there are:
- colon tumours, where there is a tumour located in the ascending colon, transverse colon, descending colon or the sigmoid
- rectal tumours, where the tumour is located less than 15 cm from the anus.
Each type requires a slightly different approach to treatment.
Symptoms
You often cannot feel cancer of the large intestine. A small amount of blood with bowel movements or abdominal cramps are not a reliable sign of large intestine cancers. These can also be caused by many other conditions.
Anal bleeding that is red may have various causes, but the presence of a malignant intestinal tumour is one of the most important ones. Uncontrolled weight loss is certainly another cause for concern. If abdominal cramps are accompanied by weight loss and/or anal blood loss, further examination for colon cancer should be started, especially if symptoms persist and/or you are older.
Changes in your bowel moment pattern (less frequent or more frequent bowel movements) and persistent diarrhoea or constipation (in spite of medication) may also be signs of a large intestine cancer.
Diagnosis and treatment
Diagnosis and treatmentPatients who wish to do so, can participate in a clinical study. Here is a list of the current studies:
The classic colonoscopy is the most widely-used detection method because not only is it highly accurate, but also because any susicious tissue found during the examination (e.g. biopsies or polyps) can also be removed during the test. The pathologist analyses the pieces of suspicious tissue under the microscope. This takes three working days on average.
These days, screening for colon cancer is also carried out with a stool test.
Usually, there is a gradual growth with damage to part of the intestinal wall and then the entire wall. When cancer cells become detached from the original tumour and penetrate deep enough to reach the blood and lymph vessels, they can escape and colonise glands. If a detached clump of cancer cells nest within another part of the body, the cancer is said to have spread or ‘metastasised’. Large intestine cancer cells sometimes end up in the liver or lungs. The stage is determined based on a global system: the TNM classification (Tumour Node Metastasis). This looks to see whether the tumour has grown through the intestinal wall (T), and if the lymph nodes have been affected (N) and when whether they have metastasised (M).
The most common treatment for cancer of the large instestine consist of oncological surgery, radiation therapy, chemotherapy and targeted therapy.
The attending physician may ask a patient to participate in scientific research (also called a clinical study or trial). For patients, participation in a study often represents an additional treatment option. In clinical trials, physicians test whether a new drug or treatment is safe and produces better results than existing treatments. However, a patient will only participate if he or she provides his or her express consent.
Treatment centres and specialisations
Treatment centres and specialisations
Latest publication date: 02/08/2024
Supervising author: Dr Monsaert Els
Something wrong or unclear on this page? Report it.
Supervising author: Dr Monsaert Els








