Varicose veins
Symptoms and causes
Symptoms and causesWhat is it?
Varicose veins are caused by malfunctioning valves in the veins of the legs. Usually, the blood in the veins of the feet flows back to the heart. Functioning valves prevent the blood from going the wrong way and flowing back towards the foot. If valves do not work properly, the blood does flow back to the foot. As a result, the veins expand due to the overpressure of the blood. This is how varicose veins are formed.
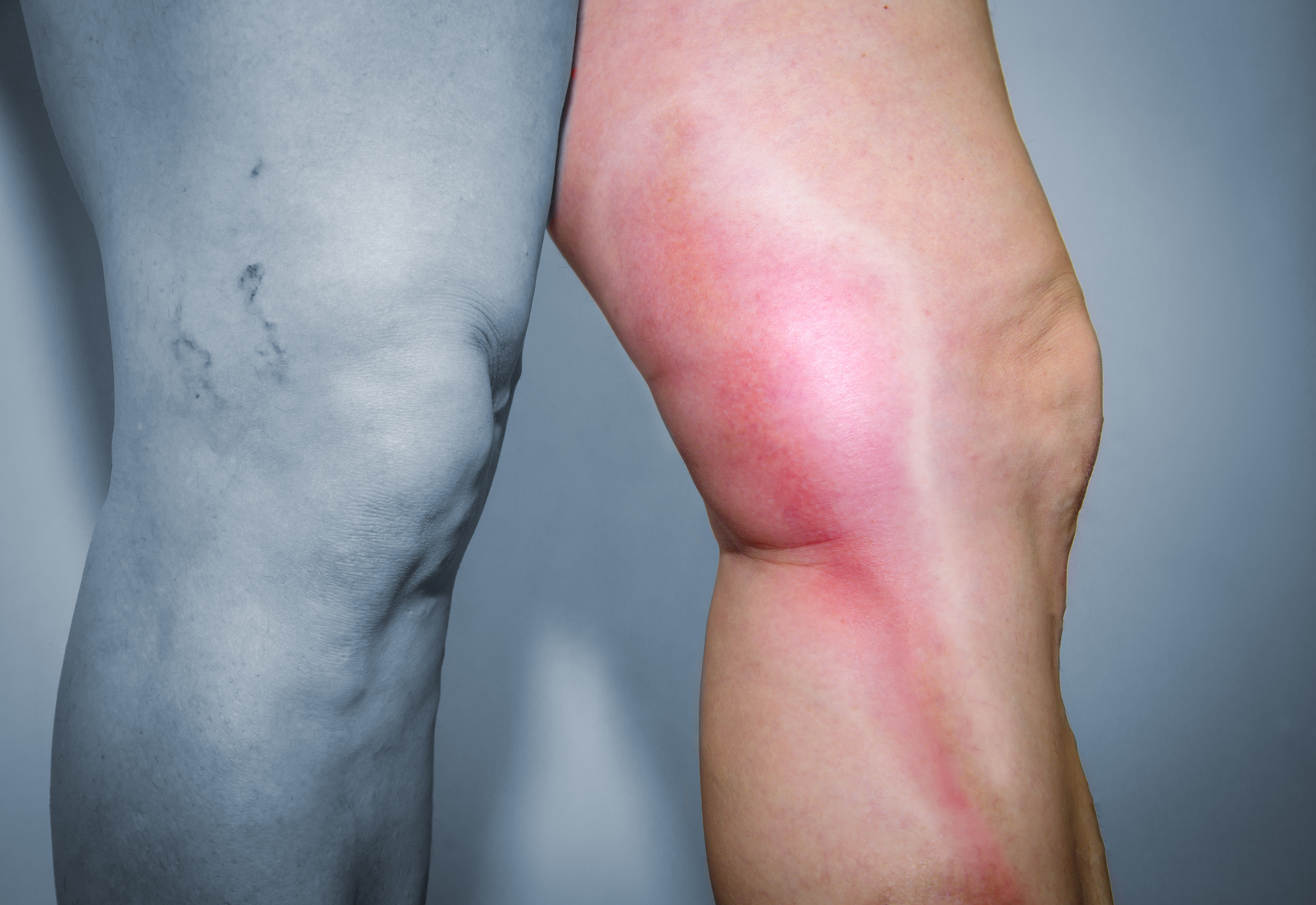
There are different forms of varicose veins (see photos):
- Limited varicose veins: varicose veins are blue or purple lines without thickening. They are also known as cobwebs or telangiectasia. These varicose veins are mostly an aesthetic nuisance and cosmetically they are easy to treat.
- Realvaricose veins: these varicose veins are cord-shaped. They lie on top of the leg and form (often very tortuous) nodules. Varicose veins usually become larger over time.
- Extensive varicose veins: advanced varicose veins are accompanied by swelling, thick legs or feet and skin abnormalities.
- Open wounds: very advanced varicose veins can cause open wounds at the level of the ankles or lower legs.




What are the symptoms?
- Clearly visible veins (cosmetically perceived as bothersome)
- Oedema/swelling
- Tired, heavy legs (possibly accompanied with cramps)
- Tingling, itching, glowing
Risk factors
- Heredity: varicose veins often run 'in the family'.
- Age: varicose veins usually do not develop until middle age.
- Gender: varicose veins are more common in women (e.g. due to pregnancy, hormones, the pill).
- Overweight: varicose veins are common in overweight people.
- Standing or sitting professions: varicose veins are more common in people with a sitting profession.
Complications
Varicose veins are not dangerous, but they can give rise to complications.
Some changes may occur in the skin:
- brown discolouration of the skin (ochre dermatitis)
- skin hardening (lipo- and dermatosclerosis)
- scarring skin (atrophy blanche)
- open leg wound (ulcer)
Bleeding from a varicose vein when it is injured is not exceptional.
Phlebitis is also possible: a thrombosis in a superficial vein that creates a red, painful area.
Diagnosis and treatment
Diagnosis and treatment
Diagnosis
In case of (suspected) varicose veins, we perform one or more examinations.
The most frequently performed examination is an echo/duplex ultrasound. This allows us to obtain a good picture of the veins and define a treatment strategy. This test is quick and painless
Treatment
There are multiple treatments and combinations of treatments for varicose veins or venous insufficiency. Depending on your personal situation and your own wishes, you and your physician will choose the optimal treatment strategy.
Compression stockings prevent problems, but do not heal the varicose veins.
Compression stockings offer the following advantages.
- They push the blood in the legs from the bottom up.
- They prevent moisture (oedema) from accumulating.

There is no medication that makes varicose veins disappear, but the medication does offer the following advantages:
- better blood circulation
- fewer symptoms
- improved valve function
This technique generates heat using radio waves (sound) with the aim of removing the very small and often red varicose veins.
During this therapy, an etching fluid (foam) is injected into the vein. This fluid irritates and damages the blood vessel wall with the aim of making the varicose vein disappear. This is mainly used for small veins (telangiectastia), but can also be useful for larger branches (convolutes).

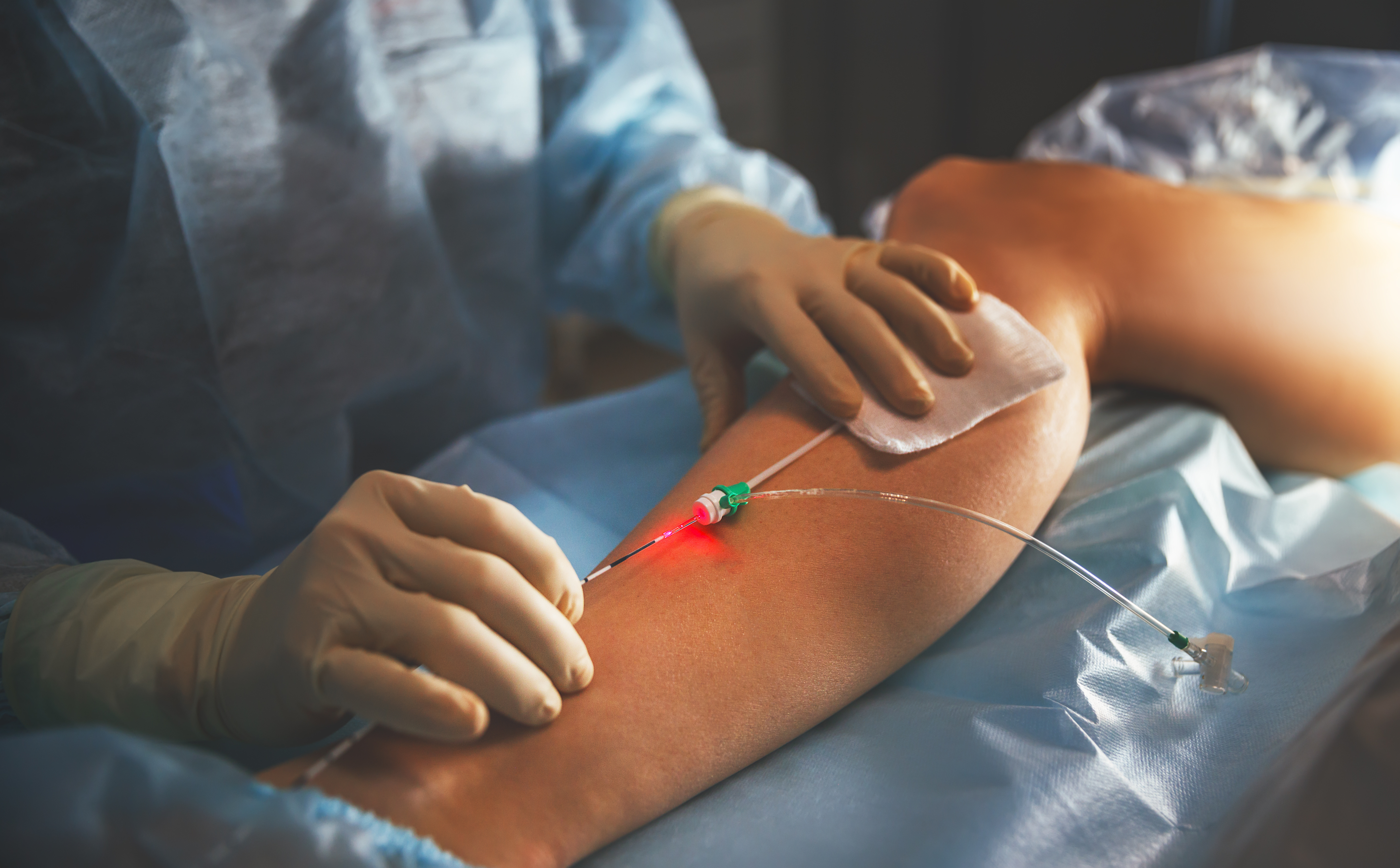
This involves treating varicose veins from the inside with a laser or radio frequency ablation (ELVeS). This technique is used for the larger trunk veins that run to the knee or groin fold.
Varicose veins can also be surgically removed via stripping or staged excisions. This technique is also used for the larger trunk veins that run to the knee or groin fold.
Treatment centres and specialisations
Treatment centres and specialisations
Latest publication date: 02/08/2024
Supervising author: Dr Willaert Willem
Something wrong or unclear on this page? Report it.
Supervising author: Dr Willaert Willem






