Breast reconstruction
What is it?
What is it?An amputated or disfigured breast causes significant damage to a woman’s self-image. Breast reconstruction may help process such loss. If a breast cancer diagnosis comes as a surprise, a conversation about the possibilities of breast reconstructions often provides something to focus on during the subsequent treatment. More and more often, the patient can choose when the breast reconstruction happens.
You can either opt for immediate breast reconstruction or for reconstruction at a later date. In immediate reconstruction, the entire surgical treatment of breast cancer (mastectomy and breast reconstruction) is performed during the same operation (and period of hospitalisation). The most important advantage of this technique is that the patient is spared the disfiguration of breast removal and wakes up from the general anaesthetic with a breast, albeit a reconstructed one. It also only involves one recovery period. The aesthetic results of immediate reconstruction are generally also the best, because the original skin envelope of the breast can be retained. However, some women find an immediately reconstructed breast somewhat more difficult to accept in the first months. Somebody who has lived with the disfiguration of breast removal for some time finds it generally a lot easier to accept the reconstructed breast.
Some women prefer to process the breast cancer diagnosis and the treatment before considering reconstruction. For these patients, delayed reconstruction (at least three to six months after completing treatment) is a better option.
If you consider immediate reconstruction, you need to know that a reconstructed breast will not alter the follow-up of breast cancer or make it more difficult. The need for follow-up treatment after mastectomy (radiotherapy - chemotherapy) is not a contraindication for immediate reconstruction. However, if radiation is necessary, then reconstruction with autologous tissue is the best choice.
At present, delayed reconstruction is still applied the most often. Yet an ever increasing number of women opts for immediate reconstruction because of the many advantages. This development is partly due to the greater accessibility and availability of information to breast cancer patients. With this in mind, a leaflet has been created. By providing an overview of the possibilities of reconstructive breast surgery the Breast Centre at the Maria Middelares General Hospital wants to assist breast cancer patients in making an informed choice.
Different techniques
Different techniquesThe range of reconstructive options can be summarised into two groups of procedures: on the one hand, techniques that use implants (internal protheses) and on the other hand, techniques that use autologous (the body’s own) tissue. The second group of techniques uses a tissue flap to reconstruct the breast, that is the patient’s tissue with its own blood supply That is why we sometimes speak of the 'warm' breast when we talk about a breast construction with its own tissue. Both pedicled and free flaps can be used for immediate breast reconstruction. The use of free flaps requires microsurgery.
The different techniques are:
- Breast reconstruction using implants
- Breast reconstruction using the large back muscle
- Breast reconstruction using a transverse rectus abdominis myocutaneous (TRAM) flap
- Breast reconstruction using DIEP flap
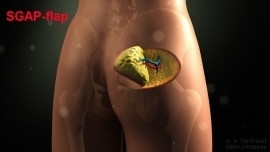
If insufficient abdominal tissue is available, skin and tissue can sometimes be removed from another part of the body to reconstruct the breast. For instance, skin and fat from the glutes can be used (SGAP flap), or from the inner thigh (TMG flap) or the outer thigh (ALT flap).
Additional techniques
Additional techniquesPost-operative phase
Post-operative phasePossible complications
No procedure is free of the risk of complications. Breast surgery also carries the normal risk of complications due to an operation, such as formation of blood clots (thrombosis), pneumonia, bleeding and wound infection. The procedure does not constitute major surgery. However, fatigue after the operation or after radiation often occurs.
If part of the breast has been removed, sometimes a dent develops. Using the new oncoplastic techniques, the surgeon will try to prevent this.
One or two thin wound drains are often placed in the surgical area to drain off blood and wound exudate. A drain in the breast can usually be removed after a few days. The underarm drain sometimes needs to remain in place for longer. After its removal, accumulation of wound exudate (seroma) may still occur. You will notice swelling and, sometimes, redness around the scar. The fluid can usually be easily removed using a syringe. In rare cases, wound healing may be slowed down by an infection. If a wound opens up, this may result in a nasty wound that takes a few weeks to heal.
Lymphoedema of the arm after axillary lymph node clearance
After breast surgery that involves the removal of the underarm lymph nodes, there is a risk of developing lymphoedema (fluid build-up) The risk of lymphoedema increases if the underarm is subjected to radiation therapy this operation. Lymphoedema may develop years after the operation. Therefore, it is important to continually pay attention to its prevention.
Centres and specialist areas
Centres and specialist areas
Something wrong or unclear on this page? Report it.
Latest publication date: 13/08/2024
Supervising author: Dr. Elzo Kraemer Ximena, Dr. Vertriest Rudolf







