Internal defibrillator (ICD/SICD) implantation
What is it?
What is it?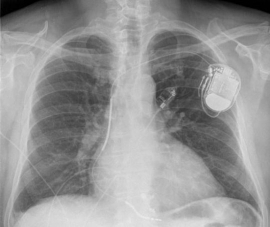
An internal defibrillator monitors the heart rhythm and intervenes, when necessary. An internal defibrillator offers supportive heart stimulation for a rhythm that is too slow and/or offers rapid stimulation or electrical impulses to interrupt a heart rhythm that is too fast.
The defibrillator system consists of:
- the defibrillator and the battery (e.g. the device itself)
- one or two pacing leads to the heart
An internal defibrillator implantation is indicated in the following circumstances:
- You have survived a period of having a heart rate that is too fast (ventricular tachycardia or ventricular fibrillation) and if a recurrent episode of this life-threatening rhythm disorder cannot be ruled out.
- Your heart problems signficantly increase your risk of sudden death. This is often as a result of heart failure and severely reduced muscle strength in the left ventricle, in spite of having received months of optimal treatment.
Physicians decide whether a classic defibrillator (ICD) or a subcutaneous defibrillator (SICD) will be chosen. See the bottom of this page for informational leaflets about both systems.
What is the process?
What is the process?Preparation
You need to have fasted: that means at least two hours for clear fluids (only water, tea and coffee), at least six hours for a light meal and dairy products and at least eight hours for a regular meal. Medication may be taken as agreed with the physician.
You will be given a surgical gown to wear. Blood samples will be collected and the nurse will place an IV line in your arm to administer medication later.
The procedure
- You will lay down on the examination table and you will have sticky electrodes placed to monitor your heart rhythm.
- Two larger adhesive patches are placed for the conduction of shocks, if necessary.
- You will be given antibiotics through the IV drip as protection against infection.
- An area of skin on the left shoulder measuring 10 by 10 cm is shaved and disinfected, and adhesive sterile sheets are placed around it. A local anaesthetic is injected to numb the skin and the underlying subcutaneous tissue. The physician makes a small incision of four centimetres.
- A small vein between the muscles is identified that allows for the delivery of one or two electrodes to the heart. If the blood vessel is not sufficient, the physician pricks a larger vein under the collar bone.
- The electrodes are placed in the right heart cavities and the contacts are checked for quality. Once the pacing leads are secured, a space is created under the skin for the defibrillator.
- The anaesthesiologist will come to put you to sleep for a while. A fast heart rate will detected and treated by a discharge from the implated device, to test whether your device is functionally optimally.
- The skin is closed with absorbable sutures and the wound is covered with a plaster. The procedure takes approximately one hour.
Aftercare
If all checks are satisfactory on the following day, you may go home. To prevent infection the plaster will stay in place for a few days. Do not shower or bathe in the first week. Avoid too much movement of the shoulder girdle.
What are the risks?
What are the risks?- Local bruising is possible but does generally not require much looking after.
- When opening the deep vein, the lung may be accidentally punctured, resulting in a collapsed lung. Radiography is therefore always performed after the procedure to detect this.
- In very rare cases, the wound gets infected despite the precautions taken. Sometimes, antibiotics must be administered and/or the device must be removed.
- In the first weeks after the procedure, the electrodes may migrate. In this case, another procedure is required.
Results
ResultsWith an internal defibrillator, you have optimal protection against adverse consequences of having a rapid heartbeat. You may still experience palpitations or fainting, but the device will stopthe heart rhythm disturbances.
Additional follow-up
- One month after the implantation, you will come to the outpatients clinic for a check-up.
- After that, you will come very six months to the clinic for further follow up.
- Follow-up also can ge given using telemonitoring.
- The defibrillator battery can provide up to ten years of support, depending on the intensity of use. Regular follow-up will indicate when the pacemaker should be replaced.
Leaflet
LeafletSee the leaflet below for more information.
Centres and specialist areas
Centres and specialist areas
Something wrong or unclear on this page? Report it.
Latest publication date: 07/08/2024
Supervising author: Dr Provenier Frank






