Knee replacement
Placement of a knee prosthesis
Placement of a knee prosthesis
The knee joint
The knee joint is formed by three bones:
- the thigh bone (femur)
- the kneecap (patella)
- the shin bone (tibia)
The knee joint works like a complex hinge. It is an important weight-bearing joint. Muscles, ligaments, menisci and cartilage play an important role. The cartilage is responsible for effective shock absorption and mobility.
When are you a candidate for a knee prosthesis?
The most common reasons for getting a knee prosthesis are:
- wear and tear on the knee (arthrosis)
- fractures
- rheumatoid arthritis
- congenital knee defects

Goal of the knee prosthesis
The knee joint is covered with cartilage on the upper leg, lower leg and the kneecap The covering is nicely smooth and a few millimetres thick.
If the cartilage (the joint's gliding layer) is severely damaged or worn, every movement becomes painful.
The goal of placing a knee prosthesis is to:
- take away the pain
- improve knee joint stability
- improve mobility and function
Total knee prosthesis
During a total knee prosthesis, the damaged cartilage, the meniscus (cartilage layers) and the cruciate ligaments are removed and replaced by a prosthesis. The knee prosthesis consists of two metal components with a plastic (polyethylene) part in between the two. The current type that is placed is also called sliding prosthesis or surface prosthesis.
The procedure lasts an hour, on average. The surgery usually follows the same process:
- The patient is brought to the operating theatre and the necessary equipment is prepared.
- A tourniquet is sometimes applied around the thigh to prevent blood loss during the procedure. The operation is performed under strict sterile conditions to minimise the risk of infection.
- The knee is usually opened with a central incision.
- The knee muscles and ligaments are usually saved.
- The damaged cartilage is shaved away at the upper and lower leg.
- A prosthesis is then placed. Careful checks are carried out to make sure that the prosthesis fits the bone.
- The proper alignment of various parts is important. They should fit together in just the right way to ensure good knee stability. Only then is the definitive prosthesis placed and fixated with cement.
- Local pain medication (LAI, local anaesthetic injection) is injected when the wound is closed.
- The wound is closed with staples and then covered with a sterile, absorbent and skin-friendly bandage.
For more info and any video recordings regarding the procedure, you can always contact your attending physician.
Possible complications
There may be complications after the procedures. Your orthopaedic surgeon will do everything possible to minimise the risk of complications.
- Post-bleeding: which may give rise to a haematoma (bruise).
- Fever: a fever may develop a few days after the operation.
- Infection: you will be given antibiotics to prevent infection.
- Phlebitis, deep vein thrombosis and pulmonary embolism: you will be given the appropriate anticoagulants (= anticoagulation medication).
- Nerve damage: the chance of nerve damage is very small.
- Stiffening of the knee: learning to bend the knee again can sometimes be tricky. Mobility under anaesthesia may be recommended.
How long does a prosthesis last?
How long a prosthesis lasts depends on several factors. Obesity and overuse can accelerate the wear process. If the knee prosthesis is worn out, it will need to be replaced.
With the current prostheses and surgical techniques, a prosthesis should be able to last for 15-20 years, with normal use. It may even last you the rest of your life.
Preparation for the surgery
Preparation for the surgeryPre-operative consultation with the GP
Your GP will perform pre-operative tests. Usually, an ECG (e.g. electrocardiogram, an image of your heart) is made. Blood samples will be collected, and, if necessary, an X-ray of the chest will be made. In consultation with your GP, you will stop blood-thinning medications (e.g. Marevan, Plavix, Sintrom, Ticlid and Marcoumar) for at least one week prior to the surgery. Your GP will decide which medication is the best substitute.
Preparation for the discharge
Your hospital stay will be relatively brief. If you suspect that your return home may cause problems, we suggest discussing this with your attending physician as soon as possible. Contact the hospital's Social Services before your admission to the hospital. The hospital social worker will then be able to work with your family in a timely way to look for a modified solution so that your discharge can proceed smoothly. The hospital social worker is able to provide extensive information about care and services.
It is sometimes necessary to recuperate at a Rehabilitation Centre after discharge. That should be prepared for ahead of time. Besides the prosthetic surgery department, there is a rehabilitation department in our hospital.
Admission
Admission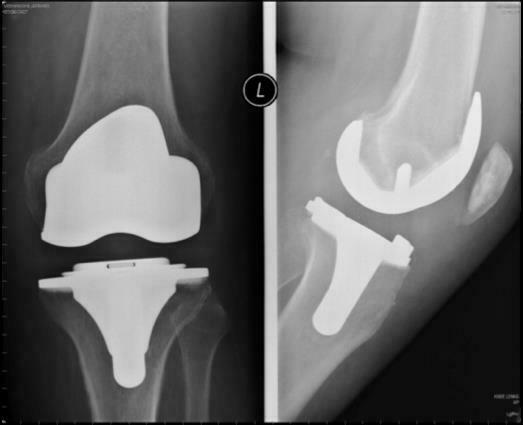
What should you take to the hospital?
- Test and examination results you have (X-rays, ECG, blood tests).
- Crutches (you can hire these from your health insurance company's lending service or from a home care organisation)
- Closed-toe, well-fitting shoes with a wide heel that give good support and plenty of room. Keep in mind that your leg or foot may be swollen for a while after the surgery.
- Current medication list
- Home medication in their original packaging
- Your identification card and blood type card
- Sleeping attire and toiletries
- Please leave valuables at home
- Forms for your hospitalisation insurance
- Forms for incapacity for work
Day of admission
On admission day, you will be expected at the appointed hour.
You will be given a identification bracelet to wear during your stay. You will be escorted to your room, receive the necessary info from the nurse who will also take your medical history (questions).
What do we expect from you?
- Please shave the surgical site the day before your admission.
- Please arrive at the hospital fasting. That means you are not allowed to eat, drink or smoke from the time your physician agreed with you.
- You should also follow your physician's guidelines on taking your daily medication on the day of admission.
- Smoking not only negatively affects your breathing during anaesthesia, but it can also negatively affect the prosthetic bone growth afterwards. Smoking is also prohibited in the hospital.
- It is also important to remove your contact lenses or glasses, dentures, hearing aids, nail polish, make-up and piercings before the operation.
When the ward nurse receives telephone notification that you are expected at the operating theatre, they will inform you and help you put on the surgical gown.
The operation
Before you are anaesthetised, the orthopaedic surgeon and the anaesthetist will visit you. Please make sure to ask any questions you may have about the anaesthesia or the operation.
The total knee operation lasts for approximately one hour and is performed while you are under anaesthesia. There are two types of anaesthesia: general anaesthesia and local anaesthesia (spinal block). The surgery is usually performed under local anaesthetics in combination with a mild form of general anaesthesia.
Pre-surgery care, the surgery itself and time in the recovery room can add up to four hours. If you are completely awake, the pain is under control and your vital signs are normal (blood pressure, pulse, respiratory rate, pain scale, etcetera), you will be brought back to the care ward.
After the operation, you will receive:
- An infusion: a thin, flexible tube will be inserted into a blood vessel to administer fluids, pain medication and antibiotics.
- A nasal cannula is sometimes necessary to administer oxygen.
- A Redonis sometimes necessary: a catheter that is placed in the wound to drain tissue, fluid and blood.
- It is sometimes necessary to rest the knee in a knee block.
Pain scale
After the operation, the medical and surgical team will do everything they can to treat your pain. The pain will be recorded on our care ward. This allows us to gain better insight into the intensity of your pain. Explaining how much pain you have is not always an obvious task. Rating it with a number between 0 and 10 can help us understand how much pain you are experiencing. In the department, a visual pain scale is used where 0 is no pain and 10 is severe pain.
Post-operative care and recovery
The day of the operation
When you come back to the care ward, you may drink and eat (a light and easily digestible lunch) as soon as you are able. You may be nauseous or need to vomit. The nurse will give you medication for those symptoms, if necessary. Your home medications can be restarted as per the advice of your physician.
You may not take any sleep medication on the day of operation. Your bandage and vital signs will be checked and recorded every four hours during the first twelve hours. You will be regularly offered an ice pack to place on the surgical site. That helps alleviate the pain and to minimise swelling.
The following day
The day after surgery, your IV and any Redon drains will be removed. The nurse will help you with going to the toilet in the morning and will help you out of bed. Your bandage will be checked daily. It will be replaced only if it is completed soaked through (with drainage from the wound or blood). During your stay, the occupational therapist and physiotherapist will work through a rehabilitation programme with you daily (except Sundays) to achieve the following concrete objectives:
- to be able to move around independently, such as in and out of bed, to the toilet, etcetera
- to take steps correctly and safely using a walker or crutches
- to walk up and down stairs safely
Exercises are necessary for a good recovery and to regain your mobility and strength in your knee. The physiotherapist and occupational therapist will start rehabilitation at the hospital and you will be given exercise instructions and advice to take home.
Discharge
DischargeYou will be ready to go home any time two to three days after the operation. This will depend on the nature of the procedure, wound healing, your general recovery and the rehabilitation. Some people, however, will temporarily stay on a Rehabilitation Department. Every patient will have X-rays taken of the knee (follow-up image). This may also be carried out at your discharge.
On the day of discharge (depending on the attending physician), your wound sutures will be taken care of and the bandage will be replaced.
You may shower with the bandage on but may not take a bath. If the bandage does not come away, leave it on until you see your GP to have the sutures removed. If your wound weeps, you may be prescribed wound care at home.
At the time of discharge, you will be given the following documents:
- a discharge letter for your GP, depending on the attending orthopaedist
- a prescription for home nursing care (if required)
- a prescription for medication
- an appointment or invitation for the first follow-up/consultation, approximately six week after the procedure
- a prescription for follow-up physiotherapy
- a medication list
Contact the attending orthopaedist if one or more of the following symptoms occur:
- sudden increase, intolerable pain
- fever
- weeping wound more than ten days after the operation
- redness, pain and warmth around the sutures
- shortness of breath
- pain in the calf
- purulent and foul-smelling discharge from the sutures
Tips for at home
Tips for at home- To get dressed, it is best to start with the leg that was operated on. To get undressed, start with the non-surgical leg.
- Listen to your body. Pain or discomfort mean that it is better to do things a bit more slowly.
- You should always have possible infections (e.g. of the urinary tract, lungs, skin, teeth...) treated immediately. Consult your physician if you have any of these, especially if you have a fever.
- It is best to not receive any injections in the site of the knee operation.
The contents of this website are only meant to serve as a guideline. The goal of this website is to inform you as much as possible about how an artificial knee is placed. Even so, you may have questions. Please do not hesitate to contact our nurses at the care ward or to contact your attending orthopaedist.
Only available in Dutch:

Brochure knieprothese
DownloadCost estimate
Cost estimateCentres and specialist areas
Centres and specialist areas
Something wrong or unclear on this page? Report it.
Latest publication date: 13/08/2024






