Cardiac resynchronisation therapy
What is it?
What is it?Resynchronisation is indicated for patients whose left and right ventricles no longer contract simultaneously. With the implant of a pacemaker or defibrillator with an extra conductor to the left ventricle the right and left halves of the heart to be stimulated simultaneously. Simultaneous stimulations ensures higher muscle strength. This has been demonstrated by echocardiography findings. In the long term, the enlarged heart may even shrink back to its normal dimensions.
Those eligible for resynchronisation therapy are patients with advanced heart failure who, despite optimum medicated treatment, have severely limited exertion tolerance due to asynchronous heart-muscle contraction.
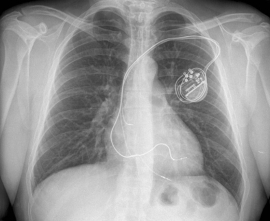
The resynchronisation system consists of:
- a device (a pacemaker or defibrillator with a battery)
- three pacing leads to the heart
Preparation
PreparationImplanting a CRT device requires a short admission (one overnight stay). After placement, you will be given an assigned room.
You will have to have fasted, as the procedure is performed under general anaesthetic. That means at least two hours for clear fluids (only water, tea and coffee), at least six hours for a light meal and dairy products and at least eight hours for a regular meal. Medication from home may be taken with a small sip of water. If you take blood thinners such as Sintrom®, Marevan® (Acenocoumarol), Marcoumar®, Pradaza®, Xarelto®, Lixiana® or Eliquis®, it is important to notify the admission nurse of the cardiology day hospital. It is also recommended to bring a list of your home medication with you to your admission. A pre-printed list is provided in the reception leaflet.
If preparatory tests are necessary, such as a blood test or EKG, these may be performed before the CRT device is implanted. The nurse will place an IV before the procedure and can administer a preventative dose of antibiotics.
Patients who are allergic to certain types of antibiotics or contrast medium must inform the nurse on admission.
Procedure
ProcedureThe device is implanted in the cardiac catheterisation laboratory. You will be accompanied to a bed in the catheterisation room and then will lie down on the examination table. The nurse will place sticky electrodes in order to monitor your heart rate during the examination. You will be asked, by preference, to lie on your left side for the CRT device implantation. The physician will mark the implantation site. The procedure is carried out under general anaesthetic, is completely painless and takes about 2 hours. In order to prevent infection, the skin at the incision site is shaved and sterilised. You will then be completely covered with sterile drapes. The skin is closed with absorbable sutures and the wound is covered with a plaster. You will wake up in the Cardiology Day Hospital and will be assigned a room. If all the checks of the device are found to be in order the next day, you may go home.
Once the pacing leads are secured, a subcutaneous space, near the shoulder, is created for the pacemaker or defibrillator. A defibrillator requires additional evaluation of the shock treatment and to that end, a high heart rate is induced. The skin is closed with absorbable sutures and the wound is covered with a plaster. You will wake up in the recovery room. The procedure takes approximately one to two hours.
If all checks of the device and the chest X-ray are found to be in order the next day, you may go home.
Risks
RisksLocal bruising is possible but generally does not require much looking after. When opening the deep vein, the lung may be accidentally perforated, resulting in a collapsed lung. Radiography is therefore always performed after the procedure to detect this. In very rare cases, the wound may become infected despite the precautions taken. Sometimes, antibiotics must be administered and/or the device must be removed. In the first weeks after the procedure, the electrodes may migrate, which will necessitate another intervention. In rare cases, the third pacing lead stimulates not only the heart but also the midriff to contract. You may sense this ‘hiccup’ more in certain positions. This problem usually disappears by reprogramming the device.
Results
ResultsCardiac resynchronisation should ensure smoother breathing, which is beneficial for your exertion tolerance. The risk of future hospitalisation due to ‘fluid in the lungs’ decreases. The number of medications can potentially be reduced, but this may only be done on the advice of your attending physician. A defibrillator also provides optimal protection against the negative effects of the accelerated heart rate. You may still have palpitations or faint, but the device will remedy the rhythm disturbance. Further follow-up will be in the outpatients clinic, in three to six-monthly consultations. Telemonitoring may also be helpful in the follow-up. Depending on the intensity of use, the pacemaker or defibrillator battery can provide up to 8 years of support. The regular follow-up will flag the need for replacement of the device.
Aftercare
AftercareTo prevent infection, the plaster will have to cover the wound for a few days; bathing and showering is prohibited during the first week for this reason. Avoid too many movements of the shoulder girdle. Since the wound is especially bruised the first few days, and may feel painful, you can still take the recommended daily dose of pain medication if needed. It is important to monitor your weight: the resynchronisation can cause you to produce quite a bit of urine. The day after the implantation, a follow-up chest X-ray will be made in order to check the position of the electrodes. The device can be checked the day after and programmed by the cardiologist.
You will receive an identification card for your CRT device. Take care to make sure you ALWAYS have this card with you.
Depending on the reason for the placement, you may drive after one to three months. Your physician will let you know which period of time is applicable to your situation.
If you come close to a magnet, the device emits a sound. This varies from a beep to a continuous sound. Distance yourself immediately from the magnet in question and contact your heart centre.
Leaflet
LeafletOnly available in Dutch:

Cardiale Resynchronisatie Therapie (CRT)
DownloadCentres and specialist areas
Centres and specialist areas
Something wrong or unclear on this page? Report it.
Latest publication date: 13/08/2024
Supervising author: Dr. Provenier Frank





